In my previous post I discussed chicken pox, and why it’s not just a harmless childhood illness. This was personal to me, because of what Shingles did to my grandmother, as well as my own odd history with chicken pox. However, this post (and the next) deals with my experiences with the death and destruction caused by unvaccinated children and adults that I have encountered professionally (mostly during my education and training). Again, as an orthopaedic surgeon it is not often that I even enter this realm that primary care physicians (mostly pediatricians) must endure daily.
Meningococcus Wasn’t Even on Their Radar
The first time (and one of the only times) I actually witness a death of a patient first hand was as a third year medical student, on my pediatrics rotation, in the pediatric ICU. The patient was a 13 or 14 year old boy who was transferred from a small outside hospital to our university medical center. He had presented there quite ill, and apparently at first they thought he had leukemia and was presenting in blast crisis. However, he continued to deteriorate rapidly and was transferred. Unfortunately by the time he arrived by ambulance he had decompensated badly, and was in DIC (disseminated intravascular coagulation) – and was bleeding and clotting at the same time. His limbs were already ischemic and his hematocrit on arrival was 7 or 8. He coded almost as soon as they got him into a room and despite valiant efforts passed away shortly after arrival. He did not have leukemia – he had meningococcal sepsis. The same bug that can often cause meningitis in teens (and those in close quarters, and is deadly in that respect in its own right), had instead become an infection in his bloodstream and spread everywhere, causing an overwhelming infection that quickly killed a healthy teenager. This was not a case of vaccine refusal or neglect – the current vaccine for meningococcus is recommended for children around 11-12 years old, with a booster 5 years later. He was a healthy kid and was just a little overdue for a physical – he hadn’t been sick in quite some time and these things happen. But seeing the look on his parents’ faces when the diagnosis was confirmed shortly after he passed was awful. Nobody said that this was a preventable disease, but his mother said something about it and she broke down. There is no guarantee that receiving the vaccine would have changed the outcome – some people have low level immune issues that can take years or decades to surface. Sometimes your body just doesn’t mount an appropriate response to a vaccine – we know they aren’t 100% effective, which is why for highly contagious diseases like measles we rely on the concept of herd immunity.
I saw the aftermath of a similar case when I was a resident. A slightly younger child had the same disease – meningococcal sepsis, and survived. But because of the DIC, all four limbs became ischemic and amputation above the knee and above the elbow was required bilaterally to save his life. An unfortunate side effect of amputations through the diaphysis (shaft) of long bones in growing children is bony overgrowth. Even with the loss of growth plates the bones ‘know’ they ‘need’ to grow, and so excess bone can form at the amputation stump. This often presents as spikes of bone at the stump that cause wounds and requires revision of the amputation. There is no good solution to stop this, but it does stop after growth ceases. This child and his family would not infrequently end up in the ER with a wound from one of his limbs – which was quite difficult to deal with in a neurologically devastated child confined to a wheelchair. The vole of vaccines here? Well he was definitely younger than the 11-12 year old recommended age for the meningococcal vaccine, although I have seen quite a few expert opinions that question whether the vaccine should instead be part of the early childhood schedule. The recommendation has not yet changed, but there is evidence that like pneumococcal pneumonia, herd immunity plays an important role (with more children getting the pneumococcal vaccine, less adults are getting pneumonia). So even though this child may have been “too young” to get the meningitis vaccine, he still could have been protected to some degree by herd immunity.

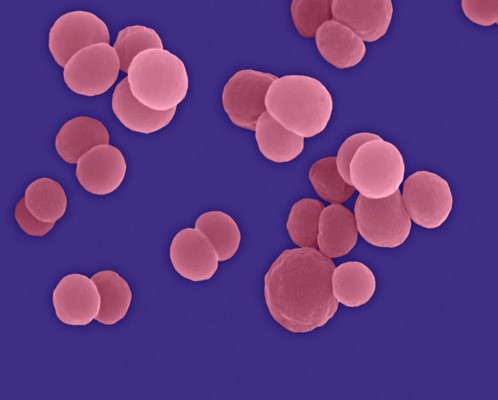
What can occur after severe meningococcal sepsis in a child
No matter the reason, this is a devastating disease, and after seeing the horrible aftermath of just one case as a medical student, I did not think I would see it rear its ugly head in my professional sphere again. I thought that was confined to ER docs, pediatricians, neurologists etc – but as I discovered its effects can spread quite far. All for a disease that we have an effective vaccine against. Since this has gotten quite long I will cover my experience with polio in part III of this post. I would venture that most recently trained physicians in the US haven’t ever dealt with the after effects of polio – but it is something that we still see in orthopaedics, although thankfully it is becoming increasingly rare.